How to leverage AI in the contact center to improve health plan member experience

By Jim Burke
0 min read
Members want channel choice, self-service, and effortless experiences. AI-powered contact center platforms enable health plans to meet rising demands.
At a time where member expectations for convenient and quality service have never been higher, healthcare payers have also seen an increased emphasis on member experience in quality ratings and in efforts to strategically differentiate in highly competitive markets.
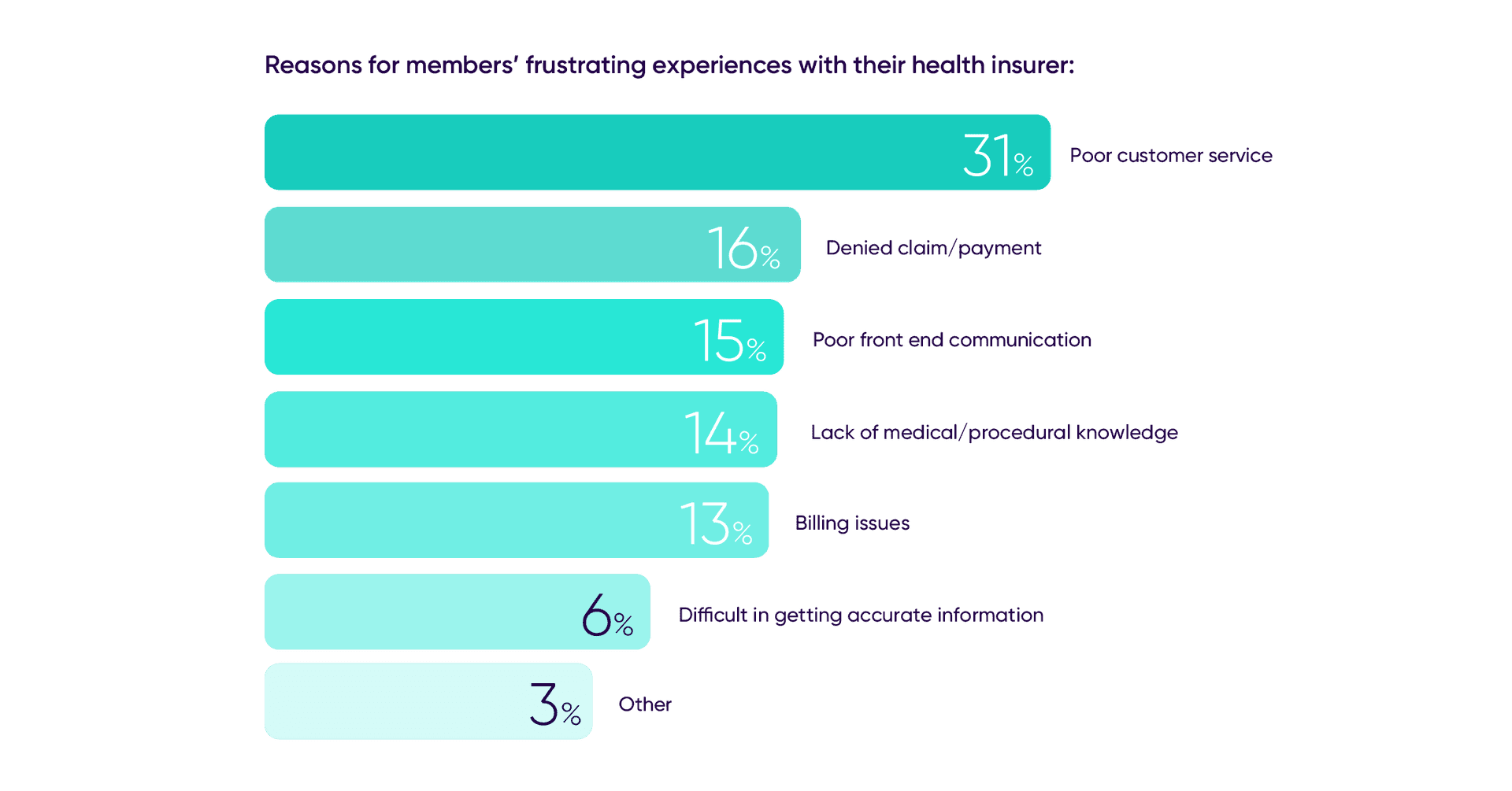
A Talkdesk Research™ report found that 78% of health insurance members say their experience was less than seamless and 28% report having had a very frustrating experience. Poor customer service, poor communication, and difficulty in getting information are just a few reasons members feel their experiences are not meeting expectations. Long call wait times were also cited as a top source of member frustration.
How can healthcare insurers change this reality and improve the member journey? AI technology in the contact center can help healthcare insurers achieve their key value drivers: member enrollment and retention, value-based care, and member experience. AI and automation for core call and chat functions have driven proven results in serving members in a smarter way.
AI is changing the way many industries operate, from product development to customer service experience, and healthcare is no exception. Keep reading to find out how AI can change the member experience and analyze the practical applications of AI-powered tools in the healthcare industry.
AI improves the agent and member experience.
There is clearly room for improvement in the healthcare member experience. Member expectations for stellar service have never been higher, and payer engagement with members is crucial to driving business and health outcomes. Members want their experiences to be:
- Consistent and connected with previous interactions.
- Tailored for every step of their healthcare journey.
- Radically convenient, allowing them to communicate anytime and anywhere.
With this in mind, how can we rethink the member experience and deliver what they expect? As the contact center continues to evolve, agents are responsible for building member relationships – they form the “front door” that serves most members’ interactions with their plan. And because members rarely call or text with their health plan when everything is going well, agents often have to support high-complexity and high-empathy conversations, which makes automation more complex.
The challenge lies in analyzing what steps of the healthcare member experience can be automated to free contact center agents from repetitive, mechanical tasks that don’t bring added value to the patient experience and support agents in high-value conversations where accuracy, empathy, and efficiency can be bolstered through technology.
Answering simple questions.
“Can I have my prescription mailed to me?” is a common member question, but not one that requires human intervention. Speech recognition technology has opened the door to building conversational AI into contact centers and healthcare providers can reap its benefits. These tools can easily replace the traditional interactive voice response (IVR) systems and the basic chatbot—giving members a technology they’ll actually enjoy using and improving their experience with the provider.
AI-powered voice and digital bots are powerful self-service tools to support members throughout simple queries and respond to this and other questions. Natural language processing (NLP) and machine learning allow members to interact with devices or services through their voice naturally and intuitively and in a highly accurate manner due to medical-grade speech recognition.
Supporting agents with real-time recommendations.
While voice and digital bots allow members to get answers to most simple questions and solve routine issues on their own, AI can also be used to empower agents to deliver differentiated service and provide impactful experiences. When dealing with more complex queries, agents can use AI recommendations and predictions to:
- Guide agents through new administrative tasks or complex queries with the latest and most accurate information.
- Educate members on important topics, like coverage and cost of care, and set up plan changes and supplemental benefits.
- Support interactions that require more complex information and a higher level of empathy using sentiment and intent detection.
AI-powered recommendations reduce the level of effort to search for information and enable agents to focus on what matters: providing a flawless, empathetic member experience.
Giving insights for proactive actions.
Members want personalized, convenient experiences and quick resolutions. Taking a proactive approach to the member journey is crucial to build stronger relationships. AI drives the next-best actions based on intent detection and real-time recommendations, leveraging agent interventions with proactive notifications. This could be a recommendation to schedule an appointment or assistance to solve administrative issues, such as helping members with claims—improving both health outcomes and service.
Reimagine the healthcare member experience.
Changes to medicare star ratings and the rise of high deductible health plans highly increase competition, turning the member experience into a differentiator. Ensure that every member interaction is tailored, unified, and convenient. Talkdesk Payer Smart Service is an end-to-end solution that delivers connected and convenient experiences by empowering staff and applying intelligent automation to the member journey.
Talkdesk Payer Smart Service enables providers to elevate member experience—through customized, seamless experiences—to stand out from the competition.
Before you go.
The success of payers depends on their ability to elevate the member journey and provide tailored and convenient experiences. For that, payers need modern, scalable contact centers and agile platforms that improve agent performance, boost engagement, and use the member experience as a competitive advantage.
To learn more about how payers can use AI to improve member experience:
- Read Why payers need to create superior health plan member experiences.
- Take a look at our datasheet for Talkdesk Payer Smart Service.
- Request a free demo today to see how Talkdesk can help you provide a superior member experience.